What is compassion-focused therapy?
Compassion-focused therapy (CFT) is an evidence-based psychological intervention that aims to increase self-compassion and to reduce self-criticism and shame (Craig, Hiskey and Spector, 2020).
Self-criticism and shame have been found to be associated with a range of mental health difficulties, including depression, anxiety, eating disorders, various personality disorder diagnoses, post-traumatic stress disorder (PTSD) and psychosis (Kannan and Levitt, 2013; Kim, Thibodeau and Jorgensen, 2011). The CFT approach is informed by multiple areas of research and theory, including evolutionary psychology, developmental psychology, social psychology, cognitive and behavioural science, neuroscience and Buddhist philosophy. Research indicates that CFT may have significant positive effects on psychological distress, depression, anxiety and stress (Beaumont and Martins, 2015; Craig et al, 2020).
CFT is an approach that is helpful for different age ranges across the life span, as well as for parents, care-givers and mental health professionals.
What is compassion?
Even the word “compassion” may be emotionally loaded for us and bring up beliefs and associations that we may have inherited and developed throughout our lives. These may include blocks we experience in accessing compassion for ourselves and others, such as beliefs that compassion is something we offer to others but not ourselves; is indulgent; or would result in a poorer work ethic or output.
We might also associate compassion with kindness, empathy, warmth and understanding. Compassion, however, may at times, involve being strong and doing what is needed, which can be “unpopular” or difficult, such as in setting boundaries in your relationships - the proverbial “putting your own oxygen mask on first”.
In CFT, the definition of compassion that we use is “a sensitivity to suffering in self and others, with a commitment to try to alleviate and prevent it” (Gilbert, 2009). This definition importantly consists of two parts. The first part goes towards suffering; that is, trying to understand our suffering and that of others with sensitivity and empathy. The second part involves committing to doing something about it. In order to develop more compassion and reduce suffering in our lives, we cannot have one without the other. If we only noticed and engaged with our suffering (the first part of the definition), we would be left in a lot of pain and unease. If we only worked on trying to alleviate or prevent suffering (the second part of the definition) without first developing an understanding, we would not know what we are working on and we may feel like we are trying everything we can, but getting nowhere.
Though there are many attributes, traits, and characteristics of compassion, in CFT we focus on three key qualities of compassion: wisdom, strength, and caring commitment.
Wisdom
Wisdom refers to the wisdom that we each have and that comes from experience. It is an understanding of what it means to be human and the universality of some of the difficulties we experience, such as the “tricky brains" that we are born with. This wisdom understands that we did not get to choose much of what we have experienced, the nature of our lives and how our past experiences have shaped us; they are not our fault.
Strength
Strength relates to fortitude and courage. It is not an aggressive power, but a source of inner confidence and authority that comes from wisdom and experience. This strength helps maintain our commitment and determination to face and heal suffering.
Caring commitment
Caring commitment speaks to a commitment to facing, rather than turning away from, life’s challenges. This involves recognising that, even though we did not cause many of our struggles and difficulties, it is our responsibility to alleviate our suffering. To commit to ourselves in a caring way involves not condemning or blaming ourselves, but rather recognising that we are each doing the best we can to move forward in what is often a difficult and complex situation.
What is the 3 Circles model?
CFT is focused on helping individuals to better understand their emotions and to relate to their emotions from a more compassionate stance. It also aims to help individuals to move out of unhelpful emotional patterns or loops that were shaped by early experiences, but that may no longer be adaptive in our current circumstances. In CFT, three main emotion or affect regulation systems are recognised, each of which motivates us toward meeting a particular set of needs.
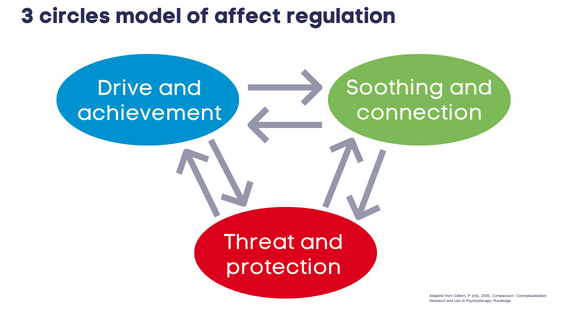
This is known as the “3 Circles” or “3-Systems” model, made up of:
- our threat and protection system
- our drive and achievement system
- our soothing and connection system.
The function of our threat and protection system is to protect us from dangers in our physical and social worlds. Our threat-based emotions (including fear, anger, disgust, guilt and shame) motivate us toward coping responses that have evolved to keep us safe, including fight, flight, freeze and appease. The threat and protection system operates on a “better safe than sorry” principle, and, hence, can at times become activated when there is no real danger present.
The function of the drive and achievement system is to motivate us to pursue goals (such as reproduction) and obtain resources (such as food, shelter, and warmth) that we need to survive. Drive-based emotions include excitement, lust, satisfaction, pride and joy, and we tend to feel quite energised, focused and productive in this system.
The function of the soothing and connection system is to help us to rest and digest, and to live in relationship with others. This system produces emotions that allow us to feel content, calm and safe around other people. Our soothing and connection system helps us to regulate the other two systems so that we don’t become exhausted or burned out.
One of the key aspects of these emotional systems is that they are shaped by experience, or what we refer to as emotional learning. For example, if we experience a situation that is threatening, our threat and protection system becomes highly alert to the possibility of this occurring again. And if we grow up in an environment where it is not safe to feel or express emotions, we may learn to relate to ourselves and our emotions in a critical, punitive or highly demanding way. This can lead us to feel threatened and ashamed by our own emotions and needs, leading to our three systems becoming out of balance, and contributing to difficulties in our mental health and overall wellbeing.
A key CFT message is that it is totally normal and human to have these three emotion regulation systems. We need to spend time in each of these systems, otherwise we wouldn’t survive. Remember, we did not choose these systems or the early experiences that shaped how we cope with being in each of these systems. Thankfully, it is possible to become more aware of what it’s like to be in each of these systems, and to learn more helpful ways to cope with and move between them.
How can CFT help your patients?
A 2018 survey by Mind, a mental health charity in the United Kingdom, found that 41% of GP consultations involve a mental health element. Given the evidence indicating that self-criticism and shame are associated with a range of mental health conditions, it is likely that a considerable proportion of patients attending your GP clinic experience difficulties with both. Those patients that will most benefit from engaging in a CFT intervention are those who present with pervasive and long-standing self-criticism, self-attacking or self-loathing. They also may present with low self-worth, or judge themselves against excessively high standards. Often, these difficulties are associated with high levels of shame and anger or disgust with oneself, as well as with difficulties with self-compassion, and with feeling soothed, safe and cared for.
There are some instances where a CFT intervention might be a good fit, but where another intervention might need to be considered before CFT. For example, where a patient is struggling with active suicidality or self-harmful behaviour, they may initially require access to an approach such as Dialectical Behaviour Therapy (DBT) to increase distress tolerance skills before engaging in CFT. Where a patient is struggling with an addiction, eating disorder or active psychosis, they may initially benefit from more specialist therapeutic treatment of same. Indeed, CFT itself has been adapted to address specific difficulties like eating disorders (Goss and Allan, 2014), hearing voices (Heriot-Maitland et al, 2019) and complex trauma (Lee and James, 2013), with a growing body of research indicating its effectiveness in these areas.
Is CFT available at SPMHS?
At SPMHS, we have been running a transdiagnostic CFT group programme since 2014, and feedback from group members and staff teams working with service users who attend the programme has been extremely positive. CFT group interventions more specifically aimed at a particular mental health difficulty, as mentioned above, are also offered by our Psychology Department. For example, a service user with psychosis who is ready to engage in therapeutic work may benefit from initially engaging in a targeted, CFT-based intervention such as the Living Through Psychosis group programme, and may later benefit from engaging in a more transdiagnostic CFT group intervention.
If you feel that our transdiagnostic group-based CFT programme or any of our focused CFT interventions offered may benefit one of your patients, please bear in mind that they would need to be under the care of a consultant at SPMHS in order to be referred to the programme. A referral to the CFT group programme could then be made by their multidisciplinary team (MDT)’s psychologist at SPMHS. Please see here on making a referral to our services.
Can you apply CFT to yourself as a GP?
From a CFT perspective, it is as important for us to be aware of our own needs as clinicians and humans, as it is to focus on the needs of our service users. In fact, we’re likely to be better clinicians if we can tune into our own needs for balance and for self-compassion.
Let’s think for a moment about your experience of your own three affect regulation systems as a GP. Recent research suggests that the role of a GP is likely to involve a high amount of time in drive and achievement, and may also be triggering of threat and protection. For example, a qualitative study by O’Dowd and colleagues (2018) looked at stress, coping and psychological resilience among physicians, including GPs, in Ireland (n = 68 physicians, including 15 GPs). They found that key stressors for Irish physicians include long shifts, lack of resources and heavy workloads. Competing demands was found to be a stressor for GPs in particular.
Similarly, a qualitative study by Riley and colleagues (2017) looked at sources of stress in GPs in England (n = 47) prior to COVID-19. They found that the key sources of stress or distress for GPs included:
- work role and demands (fear of making mistakes, complaints and inquests, revalidation, appraisal, inspections and financial worries)
- the emotional aspect of the work (managing and responding to psychosocial issues, dealing with abusive or confrontational patients)
- practice culture (practice dynamics, collegial conflict, bullying, isolation and lack of support/opportunity to discuss emotional impact of the work).
More recently, a systematic review published this year by Jefferson and colleagues looked at the impact of COVID-19 on primary care doctors’ mental health and wellbeing (Jefferson et al, 2022). Some 31 international studies were included. They found that COVID-19 led to multiple sources of stress including changed working practices; risk, exposure, and inadequate personal protective equipment (PPE); information overload; pandemic preparedness; and lack of cohesion across sectors. Studies demonstrated an impact on psychological wellbeing including stress, burnout, anxiety, depression, fear of COVID-19, lower job satisfaction and physical symptoms.
These findings suggest that GPs are understandably likely to spend a lot of time moving between their drive and achievement and threat and protection systems, and perhaps less time in their soothing and connection systems. It may be helpful for you to explore what your own three systems look like and whether you feel you might benefit from finding a little more balance between them. As clinicians, it can also be helpful to become more aware of how we relate to ourselves and our emotions in our own work and lives more broadly. If we notice a tendency toward self-criticism or holding ourselves (or others) to excessively high standards, we may begin to be curious about what impact this is having on our own wellbeing and the wellbeing of others that we work with and serve. We may also begin to wonder about what it might be like to develop more self-compassion and to cultivate a more compassionate culture within our clinical practice.
References available on request.
More on GP mental health
Useful resources
Get more information and resources around CFT, recommended by our team.
CFT-related websites and talks
- Balanced Minds
- The Compassionate Mind Foundation
- Irish Centre for Compassion Focused Therapy
- Lecture series by CFT’s founder, Paul Gilbert
CFT self-help books
- The Compassionate Mind by Paul Gilbert
- The Compassionate Mind Workbook: A step-by-step guide to developing your compassionate self by Dr Chris Irons and Elaine Beaumont
CFT app
The Self Compassion App from Dr Chris Irons and Elaine Beaumont
Continue to…
New cycles of Bipolar Recovery and Depression Recovery programmes