An overview of insomnia
The DSM-5 defines insomnia disorder as:
- Complaint of sleep quantity or problems associated with falling asleep, staying asleep and/or early morning awakenings.
- The sleep problem causes distress and/or some sort of problem at work, relationships etc.
- The sleep problem occurs at least three nights per week and has been going on for at least three months.
- The sleep problem occurs despite adequate opportunity for sleep.
- Another sleep disorder does not better explain the insomnia, is not caused by effects of a substance and is not adequately explained by coexisting mental health disorders or medical conditions.
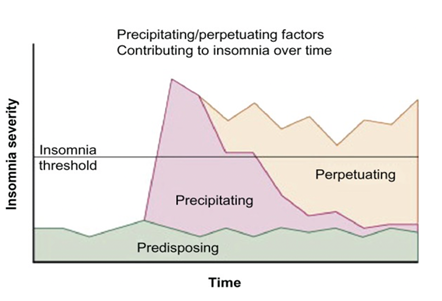
Insomnia results from three main components: 1) Predisposing factors, 2) Precipitating events, and 3) Perpetuating factors.
- Predisposing: Refer to the psychological and physiological factors that make an individual vulnerable to insomnia.
- Precipitating: What started the problem (ie. life stressors, period of illness, change in circumstances).
- Perpetuating: The cognitive and behavioural factors that maintain the problem.
The table below demonstrates that it is the perpetuating factors that keep the problem of insomnia going.
Cognitive behavioural therapy
Cognitive behavioural therapy (CBT) is based on the understanding of the connection between our thoughts, feelings and behaviours.
CBT can help us understand, challenge and change the unhelpful behaviours related to insomnia.
CBT also enables us to rethink our perceptions of ourselves, our experiences, other people and the world around us. This shift in cognition can ultimately lead to changes in how we feel and behave.

Cognitive behavioural therapy in the treatment of insomnia
Cognitive behavioural therapy for insomnia (CBT-I) is a psychological approach which is based on scientific principles and which research has shown to be effective for a wide range of problems.
Service users and therapists work together to identify and understand problems in terms of the relationship between thoughts, feelings and behaviour. The approach usually focuses on the ‘here and now’ and relies on a shared view of the problem which leads to identification of personalised, time-limited therapy goals and strategies which are continually monitored and evaluated.
CBT-I is a brief, active, structured and goal-focused therapy. Research conducted over the past 25 years has established CBT-I as the first-line treatment for persistent insomnia.
Behavioural and lifestyle considerations
Lifestyle, behavioural habits and environmental factors can influence sleep. Behavioural modification is the first stage of improving sleep.
- Daily activities: A service user’s typical day, including work commitments, exercise, meals, and leisure time.
- Wind-down routine: Calming practices to help transition from a busy day to a restful evening, such as reading, meditation, or gentle stretching.
- Sleep schedule: Consistency in timing for going to bed and waking up.
- Work routine: The organised processes and habits a service user follows during work hours to enhance productivity and maintain focus.
- Caring for others: Being responsible for the needs of others during sleep time hours.
Cognitions of sleep
- Negative thoughts about sleep can exacerbate sleep issues. Worries about falling asleep and sleep quality may lead to a poor night's sleep, creating a self-fulfilling prophecy that disrupts healthy sleep patterns.
- We often describe our sleep as “good,” “deep,” “restless,” or “hardly any sleep,” with each term reflecting our personal experiences. Assessing sleep quality is challenging, as it depends on individual perceptions.
- By reflecting on our beliefs and attitudes related to sleep; how they developed, noting how the perspective of those with insomnia differs to that of a good sleeper. How the belief in how good a day will be is largely predicated by how good a night sleep was had.
- Developing awareness of this anticipation, how it leads to efforts to control sleep, leading to associate anxious or intrusive thoughts about sleep, which are arousing and counterproductive to sleep itself.
CBT-I aims to assist service users to develop awareness of these factors and to make meaning cognitive and behavioral changes, in the following ways:
| Skill | Old way | New way |
| Balance | Bias in attention and emotion towards thoughts and behaviours related to sleep-seeking. | Allowing a sense of ‘sleepiness’ to guide sleep-related behaviour. |
| Flexibility | Rigidity in sleep-related behaviour and belief. | Adjusting to changing needs and conditions. |
| Calmness | Attachment to sleep-related needs and expectations. | Calmness stemming from non-striving and patience about sleep. |
| Commitment to values | Absorption in solving the sleep problem. | Pursuit of valued living. |
Benefits of treating insomnia
Evidence shows that CBT is an effective treatment for insomnia when co-morbid with other conditions (e.g., Harvey et al, 2015). Meaning that effective treatment of insomnia could lead to higher treatment success rates for other conditions. A study by Stott et al (2021) found a significant improvement in depression and anxiety when insomnia was treated by CBT-I; this study demonstrates the feasibility of improved outcomes in mental healthcare settings.
- Insomnia is a costly condition, known to be associated with risks related to cardiovascular diseases, obesity and diabetes, depression, anxiety and suicide, this indicates the potential mental and physical benefits of correctly treating insomnia with a therapeutic intervention.
- Untreated insomnia significantly predicts sick leave and personal finance (Baglioni et al, 2019).
- Evidence shows that CBT is an effective treatment for insomnia as the primary disorder (Morin et al, 2006; Freeman et al, 2017). CBT-I offers a treatment option to those with no previous experience of psychiatric services and who have no pre-existing mental health conditions.
- Hypnotic medication remains the dominant therapeutic modality; however this is not the recommended first-line treatment approach and has associated risks related to addiction and dependence.
- The non-pharmacological treatment of CBT-I aims to enable people to build skills for long-term sleep success and avoid any dependency and addiction.
- Insomnia is associated with considerable direct and indirect healthcare costs.
- Group-based intervention offers the opportunity for wider, less resource-intensive dissemination of the CBT-I approach, allowing multiple patients to gain at once.
CBT-I group programme at St Patrick’s Mental Health Services
A CBT-I group programme is available at St Patrick’s Mental Health Services (SPMHS), with direct referrals to the programme accepted from GPs.
The group is conducted as a therapeutic intervention, with the facilitator using CBT-informed Socratic questioning techniques to help group members to re-evaluate previous conclusions and construct new ideas. The psychoeducation content of the group covers topics such as:
- Variations and requirements of sleep
- The five sleep stages
- Predisposing, precipitating and perpetuating factors in insomnia
- Attentional bias
- Sleep hygiene
- Developing an awareness of the two systems in the body; homeostasis and the circadian rhythm
- Stimulus control
- Sleep restriction
- Relaxation techniques
- Cognitive restructuring
- Managing arousal
- Problem-solving.
The CBT-I programme at SPMHS takes place via Microsoft Teams for one-half day per week on Friday mornings for eight weeks and is facilitated by two cognitive behavioural therapists trained in the CBT-I approach to treating insomnia. CBT-I is suitable for individuals over the age of 18 who:
- Are able to attend group programmes on MS Teams
- Meet the DSM-5 criteria for insomnia, with the sleep problem occurring at least three nights per week and has been ongoing for at least three months
- Have a complaint related to sleep quality or quantity associated with problems falling asleep, staying asleep, and/or early morning wakening
- Have a sleep problem that causes distress and/or affects daily functioning
- Do not have any pre-existing sleep disorder or requirement for physical health assessment for suspected sleep disorder
- Have a sleep problem which occurs despite adequate opportunity for sleep
- Do not have a diagnosis of bipolar disorder, recent psychosis, or history of seizures
- Have insomnia that is not caused by the effects of a substance and is not adequately explained by coexisting mental health difficulties or medical conditions
- Are willing and motivated to engage in the group and make changes to their sleep routine
- May attend even if they are currently utilising medication for sleep, this can be taken in combination with CBT-I
- Have the cognitive capability to attend and engage in the group.
Referrals to the CBT-I programme at St Patrick’s Mental Health Services
Individuals do not need to be under the care of an SPMHS’ consultant to be referred to CBT-I. Please note that the referrer retains clinical responsibility for the service user while they are attending an SPMHS day programme.
Referral forms are available at stpatricks.ie/gps-referrals. You can send completed referral forms to our Referral and Assessment Service by Healthmail, by emailing it to referrals@stpatricks.ie.
Please note that upon receipt, all referrals for any programmes will be processed by St Patrick’s Mental Health Services for insurance clearance purposes.
In conclusion
CBT-I offers prescribers an alternative treatment to pharmacological interventions and has been shown to lead to lasting improvements in sleep quality. The CBT-I group gives GPs an alternative treatment option for those in their care who would otherwise rely on medication management.

